2023 Medicaid Access and Landscape Review for Sickle Cell Disease: Findings from the Assessment of Access Barriers in State Medicaid Programs
Introduction
Sickle cell disease (SCD) is experiencing an historic moment where new therapies are becoming available for patients. With new treatment options available, it is important to evaluate the role of the payer and coverage policies across the U.S., and understand their role in supporting fair access to SCD therapies. SCD patients and caregivers often report challenges that impact their ability to have timely access to care or result in a high burden of out-of-pocket costs. There is an emerging debate of whether insurance coverage is providing fair access to therapies for SCD.
As part of our commitment to expanding access and increasing advocacy opportunities, Sick Cells is working to gain insight into what factors decision makers do—and do not—consider when determining access criteria for SCD therapies. This information helps inform the broader picture of access and advocate for state efforts to improve health equity for those with SCD.
To provide context to these debates, Sick Cells conducts an annual Medicaid Access and Landscape Review to explore state and managed care documents that outline coverage criteria and answer three key questions:
- What is the current coverage status in Medicaid programs for common therapies used to manage sickle cell disease?
- How are prior authorization protocols and step therapy requirements used across state Medicaid programs?
- Do Medicaid programs provide adequate transparency into coverage criteria and decision-making processes?
An environmental scan of coverage criteria under state and managed care will be supplemented by annual survey findings and included in the full analysis. These results can serve as a tool for assessment and as the starting point for dialogue and action to achieve improved access to therapies.
Methodology
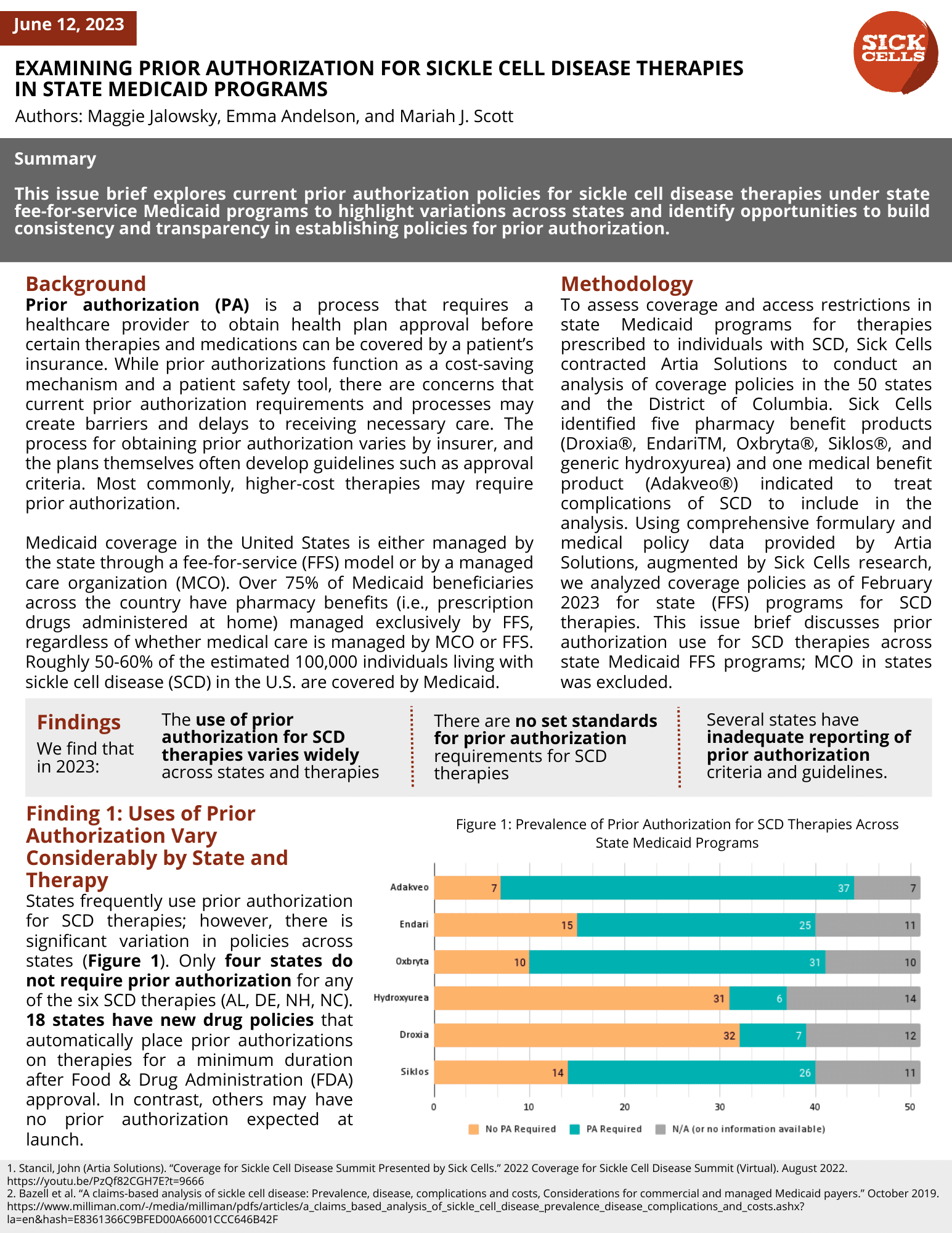
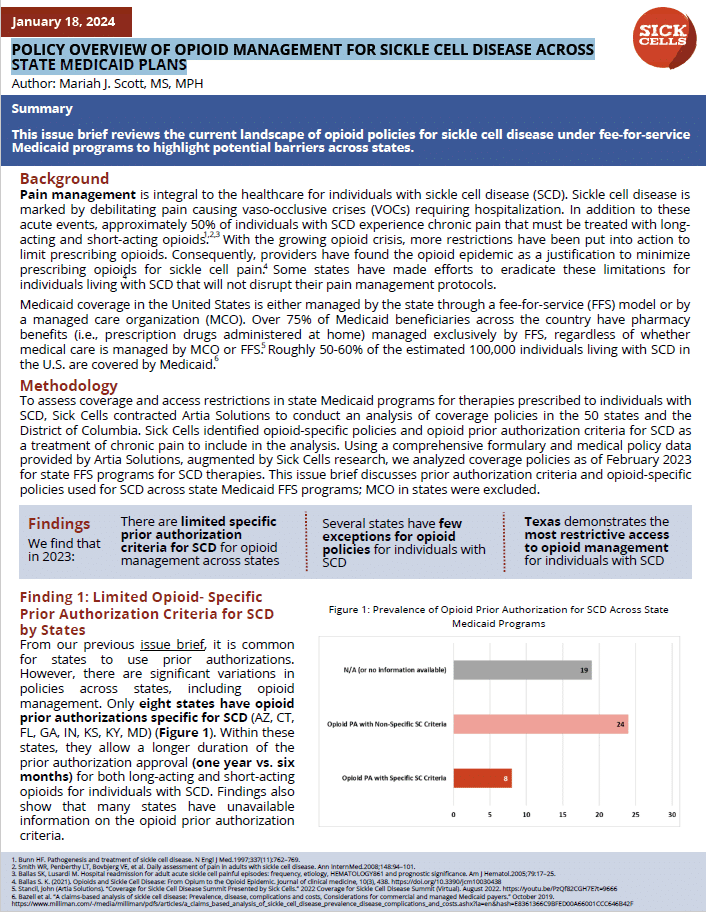
To assess coverage and access restrictions in state Medicaid programs for therapies prescribed to individuals with SCD, Sick Cells contracted Artia Solutions to conduct an analysis of coverage policies in the 50 states and the District of Columbia. Sick Cells identified commonly used pharmacy and medical benefit products indicated to treat complications of SCD to include in the analysis. Using comprehensive formulary and medical policy data provided by Artia Solutions, augmented by Sick Cells research, we analyzed coverage policies as of February 2023 for state (FFS) programs and managed care organizations (MCOs) for SCD therapies.
Key Findings and Publications
- Issue Brief #1: Examining Prior Authorization for Sickle Cell Disease Therapies in State Medicaid Programs.